Diabetic Retinopathy
What is Diabetic Retinopathy?
The retina is the layer of specialized nerve tissue lining the back of the eye that allows you to see. A healthy retina is critical for normal vision. The abnormally high levels of blood sugar associated with diabetes can cause damage to the small blood vessels that supply oxygen and nutrients to the retina. Without the proper amount of oxygen and nutrients over time, the retina can become damaged. This damage to the retinal blood vessels is called diabetic retinopathy. The disease affects half of all people diagnosed with diabetes.
What are the different types of Diabetic Retinopathy and what symptoms do they cause?
Diabetic retinopathy is classified as non-proliferative (NPDR) and proliferative diabetic retinopathy (PDR). There are various levels of severity of each kind of diabetic retinopathy and each is associated with different complications that can affect the vision. Mild diabetic damage to the retina may go unnoticed because early symptoms can be subtle, and tend to get worse over the years.
Non-Proliferative Diabetic Retinopathy
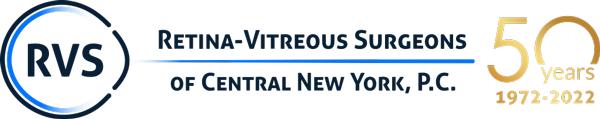
Prolonged exposure to high blood sugars damages the small blood vessels in the retina. Over time the blood vessels develop tiny weak areas called microaneurysms. These microaneurysms can rupture and leak, resulting in retinal bleeding and swelling (figure 1). These changes are collectively referred to as non-proliferative diabetic retinopathy (NPDR). In early or mild NPDR, there are very few symptoms but as the damage continues, macular edema or macular ischemia (see below) can develop and cause vision loss.
Macular edema
The macula is the part of the retina that is responsible for your detailed vision and lies in at the very center of the retina. Macular edema is swelling of the macula. In diabetic retinopathy, macular edema is caused by fluid leaking from the damaged blood vessels in the macula (figure 2). Macular edema can cause blurry vision, distortion and a small blind spot.
Macular ischemia
As a result of the poor blood flow to the macula, over time the small blood vessels (capillaries) can close off completely, causing macular ischemia. Macular ischemia causes the death of the nerve cells in the macula responsible for fine vision. This is an irreversible process that leads to a permanent untreatable central blind spot and decreased central vision.
Proliferative Diabetic Retinopathy
This is the most advanced and serious form of diabetic retinopathy. New blood vessels grow or proliferate in the eye, a process called neovascularization (figure 3). As the diabetic retinopathy advances and more and more retinal blood vessels close off, the eye responds by growing new blood vessels on the surface of the retina and over the optic nerve. These new blood vessels are very problematic because they tend to bleed and cause scaring on the surface of the retina.
Vitreous Hemorrhage
The new blood vessels that grow inside of the eye in PDR tend to bleed into the vitreous, the gel-like substance that fills the eye. The vitreous bleeding or hemorrhage can be mild, causing a few small floaters, or very severe leading to almost complete vision loss. Over time, the vitreous blood tends to clear from the eye and the vision improves. However, without treatment, bleeding tends to continue and can lead to more serious problems such as glaucoma and retinal detachment.
Tractional Retinal Detachment
As the new blood vessels associated with PDR continue to bleed they can begin to form scar tissue and start shrinking. As the new blood vessels shrink and contract they pull on the retina causing retinal wrinkling and distorted vision. If the blood vessels contract a lot, they can pull the retina off the back of the eye causing a retinal detachment (figure 5). Without treatment, the retinal detachment can easily lead to permanent vision loss.
Neovascular Glaucoma
Some eyes with advanced diabetic retinopathy respond to the loss of blood supply by growing new vessels in the front part of the eye. These vessels can grow on the iris and over the normal drainage channel in the eye, blocking fluid from draining out of the eye. Without a pathway for fluid to get out of the eye, pressure can increase resulting in severe glaucoma. This neovascular glaucoma can cause severe eye pain and lead to severe damage to the optic nerve in the eye.
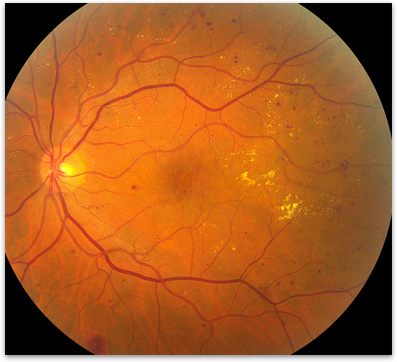
Figure 1. Non-proliferative diabetic retinopathy in an eye showing the multiple areas of bleeding and exudate.
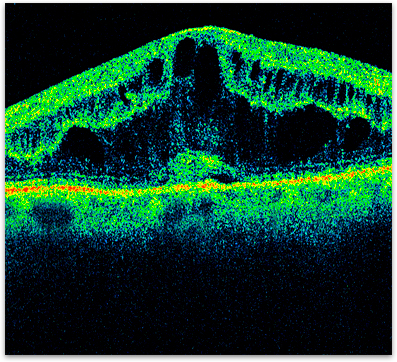
Figure 2. OCT of diabetic macular edema.
Figure 3. New blood vessels growing on the surface of the retina in a case of proliferative diabetic retinopathy.
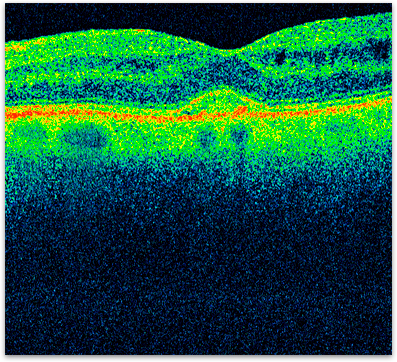
Figure 4. OCT of the same eye as figure 2 showing the resolution of the macular edema from injections of medication into the eye.
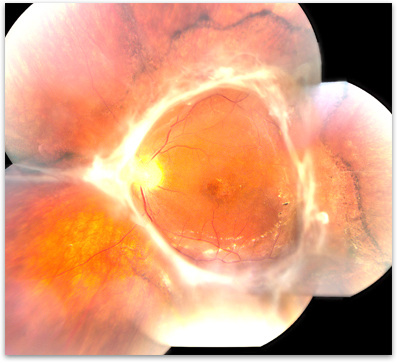
Figure 5. Tractional retinal detachment in a case of severe proliferative diabetic retinopathy.
Who is at risk for Diabetic Retinopathy?
Anyone who has diabetes is at risk for retinopathy. Diabetic retinopathy is the most common cause of blindness in the 24-70 year age group. The risk of developing diabetic retinopathy increases the longer someone has the disease. Severe damage and vision loss are much more likely to develop if the diabetes is under poor control or has been under poor control in the past. For reasons not fully understood, pregnancy can accelerate the development of diabetic retinopathy as well.
How is Diabetic Retinopathy diagnosed?
Your retina specialist can diagnose and determine the severity of the diabetic retinopathy by completing a dilated examination of the eyes. Specialized testing is often used to confirm the diagnosis and evaluate the extent of retinal damage. A photographic dye test called a fluorescein angiogram can be used to find the leaking blood vessels, identify areas of macular ischemia, and retinal neovascularization. Optical coherence tomography (OCT) is used to obtain a high-resolution cross-sectional image of the retinal structure (figure 2). This technique is useful in documenting the degree of swelling in the retina and monitoring response to treatment.
What can I do to protect my vision?
Vision loss in diabetes is usually preventable with the appropriate treatment and care. The most important thing you can do to prevent vision loss from diabetes is to monitor and control your blood sugar and blood pressure. Ideally your Hemoglobin A1C should be maintained at 7.0 or less. Optimal control of blood sugar levels slows the onset and progression of diabetic retinopathy. Every diabetic should have a dilated eye examination at least once a year.
How is Diabetic Retinopathy treated?
The most important aspect in the treatment of diabetic retinopathy is optimal control of blood sugar. Without optimal control any treatment for diabetic retinopathy is much less likely to work.
Macular Edema
Macular edema can sometimes be helped with focal laser treatment to the leaking blood vessels in the macula. Treatment is performed in the office and, in most cases slows down the rate of vision loss. Some people even have a partial improvement in the vision. Focal laser may need to be repeated if new areas of leaking blood vessels develop. In many cases medications can be injected into the vitreous cavity, either alone or in combination with laser, to treat macular edema. For most people these medications can help more than laser treatment alone but often need to be repeated, especially early in the treatment of macular edema (figure 4). Occasionally, vitrectomy surgery may be recommended to treat macular edema that is not helped by other treatments.
Proliferative Diabetic Retinopathy
Another type of in-office laser procedure, pan-retinal photocoagulation, is the mainstay for controlling retinal neovascularization. In this procedure the peripheral retina is treated extensively with laser to target the abnormal blood vessels. This technique is not intended to improve vision but rather lowers the chances of severe vision loss by up to 50%. Because the peripheral retina is treated, pan retinal photocoagulation can sometimes reduce night or side vision.
Vitreous Hemorrhage
Vitreous hemorrhage usually occurs when the neovascularization in proliferative diabetic retinopathy bleeds into the vitreous gel. This usually means that, if possible, pan-retinal photocoagulation needs to be performed. Since the vitreous hemorrhage will often resolve on its own over several weeks, immediate intervention is often not necessary. If the vitreous hemorrhage does not clear or new bleeding occurs, then vitrectomy surgery is often recommended. In this surgery, the blood and vitreous gel that fills the eye is removed and laser is used to treat the neovascularization.
Tractional Retinal Detachment
In some cases of tractional retinal detachment (figure 5), when central vision is threatened, vitrectomy surgery is recommended. The procedure involves removing the vitreous gel from the eye and then removing the scar tissue from the surface of the retina that is causing the retinal detachment. The surgery relieves the pulling effect of the scar tissue and allows the retina to lie flat on the back wall of the eye again.
Treatment of diabetic retinopathy is continuously advancing. At RVS we have been involved with the National Institute of Health funded DRCRnet since its inception. This is the most important and influential research group working on improving the quality of life for patients with diabetic retinopathy. At RVS we are on the cutting edge of medical and surgical treatment for diabetic retinopathy.
What is the long-term impact of Diabetic Retinopathy on my vision?
The prognosis for your vision largely depends on the severity of the diabetic retinopathy. Diabetic retinopathy is the most common cause of blindness in the 24-70 year age group. However, the vision loss with diabetes is largely preventable. Even with advanced forms of diabetic retinopathy, with proper treatment and care, there is a 90 percent chance of saving the vision. It is important to work with your eye care specialist and your primary care physician in order to prevent vision loss.
What can I do to protect my vision?
Vision loss in diabetes is usually preventable with the appropriate treatment and care. The most important thing you can do to prevent vision loss from diabetes is to monitor and control your blood sugar and blood pressure. Ideally your Hemoglobin A1C should be maintained at 7.0 or less. Optimal control of blood sugar levels slows the onset and progression of diabetic retinopathy. Every diabetic should have a dilated eye examination at least once a year.