Image of the Month - April 2020
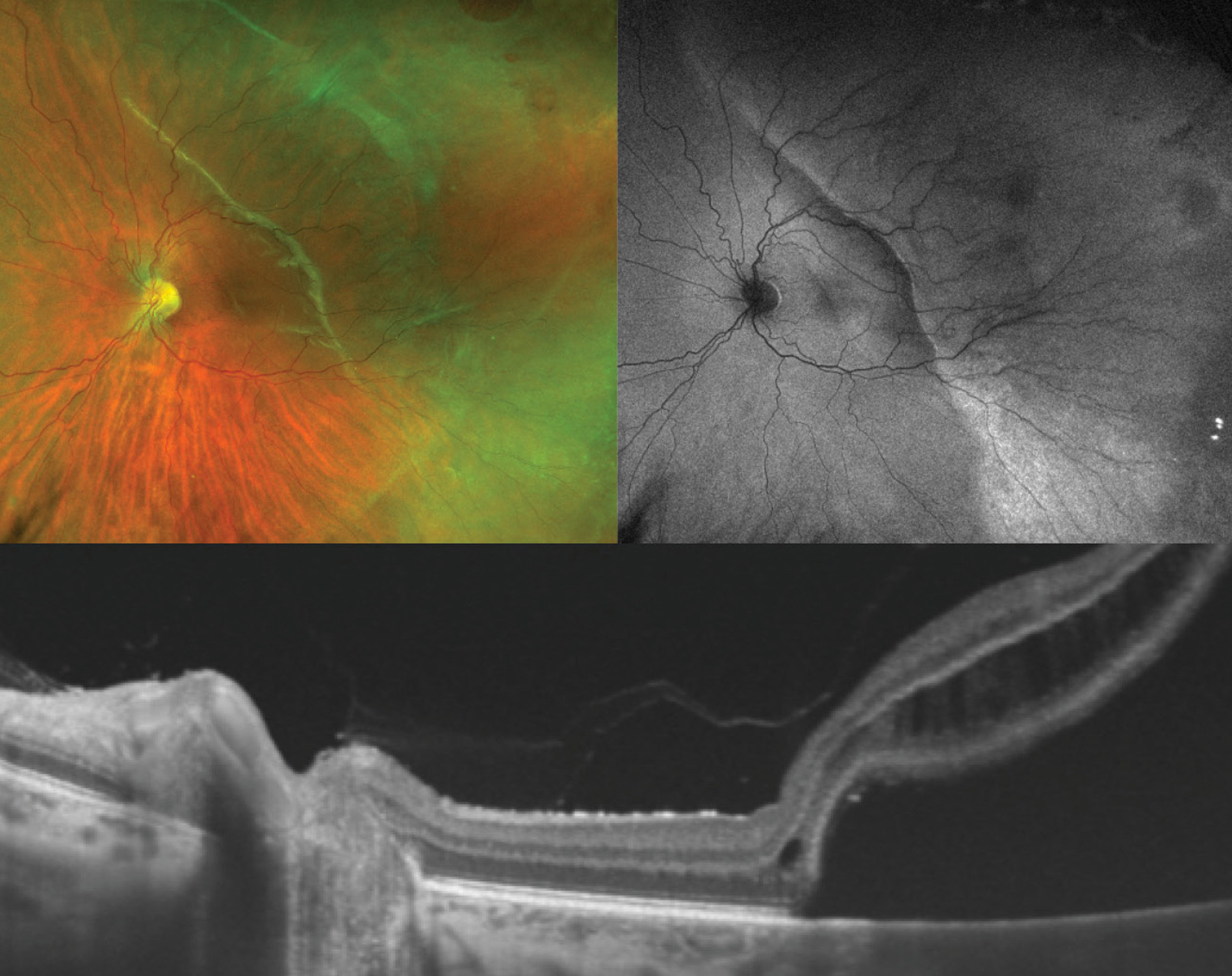
(Photo credit: Jeffrey Barker)
This multi-modal image depicts the left eye of a 33-year old patient, who was a former premature infant born at 28 weeks of gestation, with rhegmatogenous retinal detachment. The ultrawidefield fundus photograph (top left) shows a series of round retinal holes in the temporal retinal periphery, very posterior lattice degeneration, subretinal fluid as well as a demarcation line in the posterior pole. Autofluorescence (top right) demonstrates different grades of hyperautofluorescence resembling the dynamics of the subretinal fluid. One can imagine that the patient had an initial retinal detachment that was bordering to the previous demarcation, depicted by the bright autofluorescent line within the temporal macula, which subsequently progressed into the central macula and fovea region depicted by the less intense autofluorescence more nasally. This is consistent with an acute on chronic progression of retinal detachment. Further, the autofluorescence image clearly outlines the anterior extent of blood vessel growth. The temporal blood vessels, which are slightly more tortuous distally, end in zone II and the anterior retina remains immature, whereas the nasal retina is fully vascularized. Swept source optical coherence tomography (bottom) shows an attached posterior hyaloid and liquified cortical vitreous, intraretinal schisis as well as subretinal fluid abutting the nasal fovea. Given the increased survival rates of premature infants beginning in the 1970s and 1980s, adults with former retinopathy of prematurity (ROP) present a more common phenomenon. Late-complications in eyes with ROP that did not meet threshold for treatment during infancy are frequent and include lattice degeneration, retinal holes, retinal tears, severely liquified vitreous, visible vitreous condensations, peripheral tractional retinoschisis, and most concerningly retinal detachment. The patient shown here presented with a subacute retinal detachment without posterior vitreous detachment and underwent uncomplicated scleral buckling with external cryotherapy. Surgery for these eyes can be challenging, owed to the abnormal vitreoretinal interface, severely liquified vitreous, persistent avascular retina, occasional reactivated neovascularization, and extremely posterior insertion of the vitreous base. Exemplifying this, primary surgical failure is reported around 30%. Given the frequency of late ROP sequelae and their significance, patients with ROP require lifelong surveillance and their retinas should be regarded as “forever premature”.